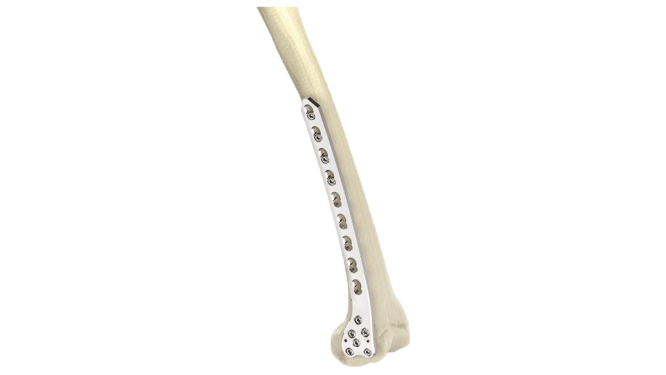
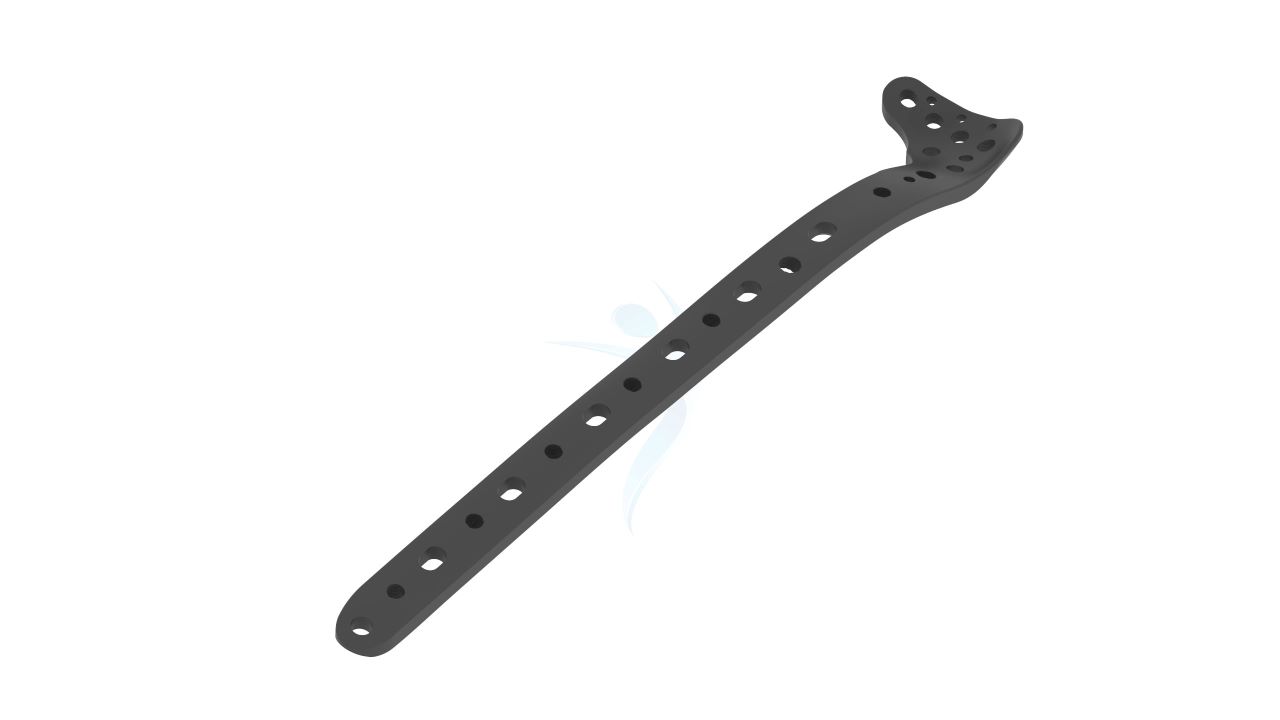
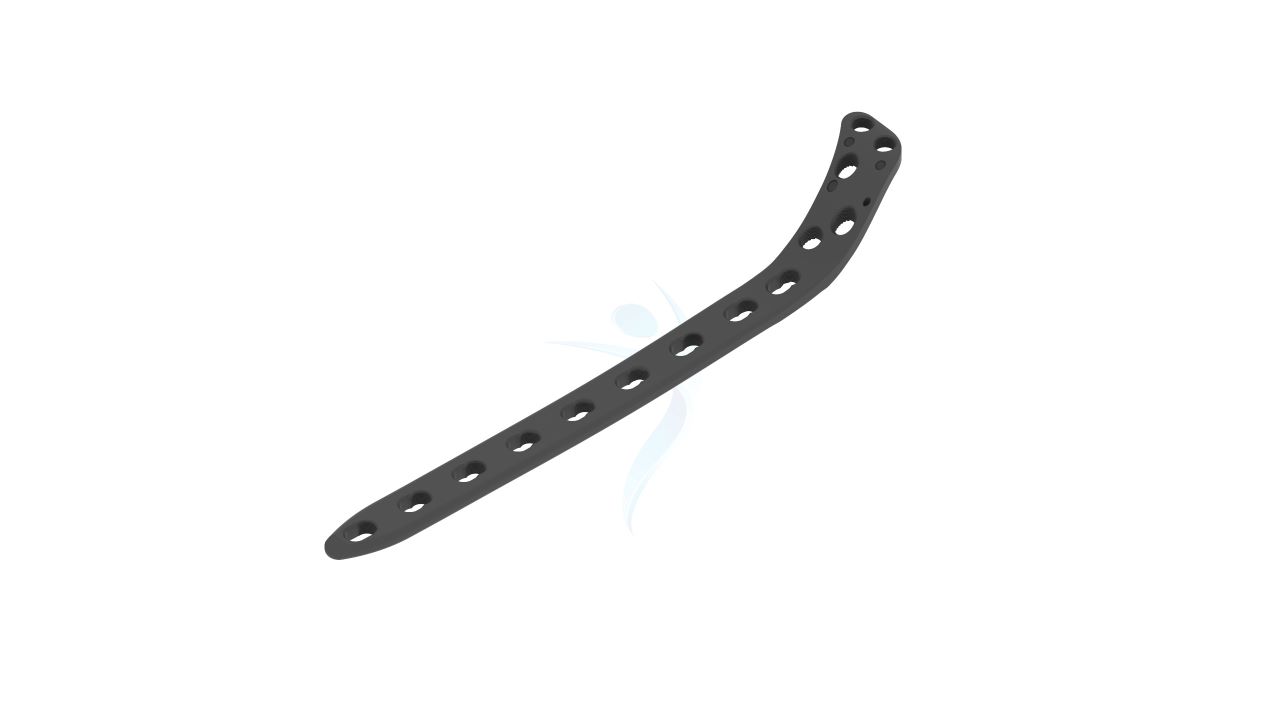
Proximal Tibia Plate 3.5 mm
Product Overview
The 3.5 mm Proximal Tibia Plate is a trusted orthopedic fixation device specifically engineered to provide stable and precise fixation for proximal tibia fractures. Crafted from high-quality,durable titanium material, this plate combines strength with biocompatibility to ensure reliable performance. It's anatomical design conforms seamlessly to the proximal tibia, offering an optimal fit and promoting proper alignment during the healing process. With versatile screw hole options, surgeons can achieve secure fixation tailored to each patient's unique needs.




Product Uses
- Proximal Tibia Fracture Fixation: The plate is utilized for stable fixation of proximal tibia fractures, providing support and alignment to promote proper healing.
- Osteotomies: In corrective osteotomy procedures involving the proximal tibia, the plate can be used to stabilize and align the bone, helping to correct deformities and improve joint function.
- Nonunion Treatment:The plate can aid in the treatment of nonunion cases, where the tibia fails to heal properly.
- Malunion Correction: In cases of malunion, where the tibia has healed in an undesirable position, the plate can be used to realign the bone and restore proper alignment and function.
- Tibial Plateau Fracture Fixation:The 3.5 mm Proximal Tibia Plate is commonly employed for fixation of tibial plateau fractures, providing stable support to the fractured bone fragments and facilitating proper healing.
Product Specification
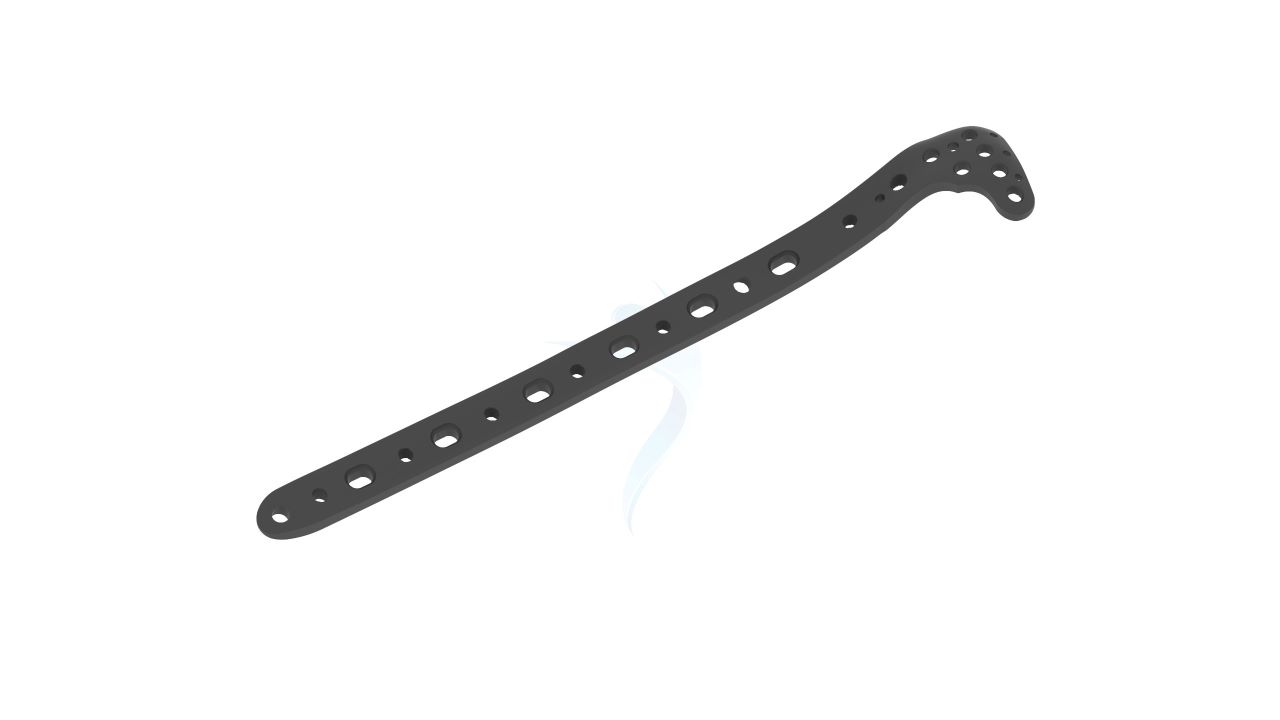
- Width: The plate has a width of 3.5 mm specifically designed for applications requiring a compact yet robust fixation solution for the proximal tibia.
- Material:The plate is made from high-quality stainless steel or titanium alloy. These materials offer strength, durability, biocompatibility, and corrosion resistance.
- Anatomical Design: The plate is anatomically contoured to match the shape of the proximal tibia bone, allowing for proper fit and alignment.
- Sterility: 3.5 mm Proximal Tibia Plates are typically supplied sterile and individually packaged to ensure product safety and reduce the risk of contamination.
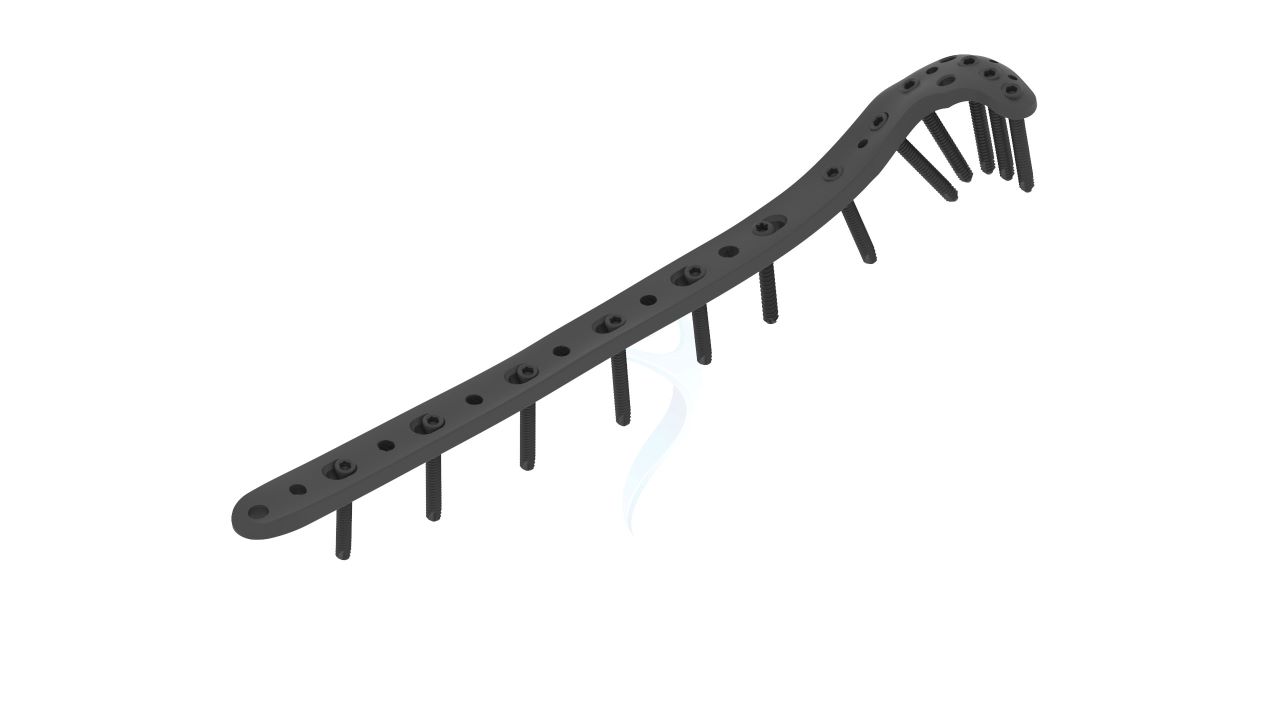
- Screw Holes: The plate features multiple screw holes of various sizes and configurations. This provides flexibility in screw placement to accommodate different fracture patterns, bone quality, and surgical techniques.
3.5 mm Proximal Tibia Plate Sizes
Comprehensive Guide for Proximal Tibia Plate 3.5 mm (ASLP)
- Medical Evaluation : Prior to the surgery, a comprehensive medical evaluation will be conducted to assess your overall health and suitability for the procedure.
- Surgical Consultation : You will have a consultation with your orthopedic surgeon to discuss the specific details of the surgery, including the use of the 3.5 mm Proximal Tibia Plate.
- Pre-operative Instructions : Your surgeon will provide specific pre-operative instructions, which may include guidelines regarding eating and drinking prior to the surgery, medication management, and instructions for any required fasting.
- Medication Review : It is essential to inform your surgeon about any medications you are currently taking, including prescription medications, over-the-counter drugs, and supplements.
- Anesthesia Consultation : If general anesthesia or regional anesthesia (such as a nerve block) will be used during the procedure, you may be required to have a separate consultation with an anesthesiologist to evaluate your anesthesia options and address any concerns.
- Anesthesia Administration : The surgery is typically performed under general anesthesia, which means you will be asleep and pain-free throughout the procedure. Your anesthesiologist will administer the anesthesia and monitor your vital signs during the surgery.
- Incision : The surgeon will make an incision over the affected area of the proximal tibia. The size and location of the incision may vary based on the specific fracture pattern and surgical approach chosen.
- Fracture Reduction : The fractured bone fragments will be carefully repositioned (reduced) into their anatomically correct alignment.
- Plate Placement : The 3.5 mm Proximal Tibia Plate will be positioned on the lateral aspect of the proximal tibia, spanning the fracture site.
- Screw Insertion : The surgeon will insert screws through the plate and into the bone to secure the fracture fragments.
- Hospital Stay : After the surgery, you will be monitored in a recovery area until you are stable and awake from the anesthesia. The length of your hospital stay will depend on various factors, such as the extent of the surgery and your overall health.
- Pain Management : Your healthcare team will provide pain medications to keep you comfortable during the recovery period. Follow the prescribed pain management regimen and notify the healthcare provider if you experience excessive pain or have concerns.
- Wound Care : Proper wound care is crucial for preventing infection and promoting healing. Your surgeon will provide specific instructions on how to care for the incision site, including when to change dressings, how to keep the area clean, and any signs of infection to watch for.
- Immobilization and Weight-Bearing : Depending on the specific fracture and surgical approach, you may require immobilization of the leg using a cast, brace, or splint. Your surgeon will advise you on weight-bearing restrictions and the use of crutches or other assistive devices.
- Follow-up Appointments : Your surgeon will schedule regular follow-up appointments to monitor your progress and assess the healing process. These appointments are essential for removing sutures or staples, evaluating the stability of the implant, and adjusting your treatment plan if necessary.





.png)