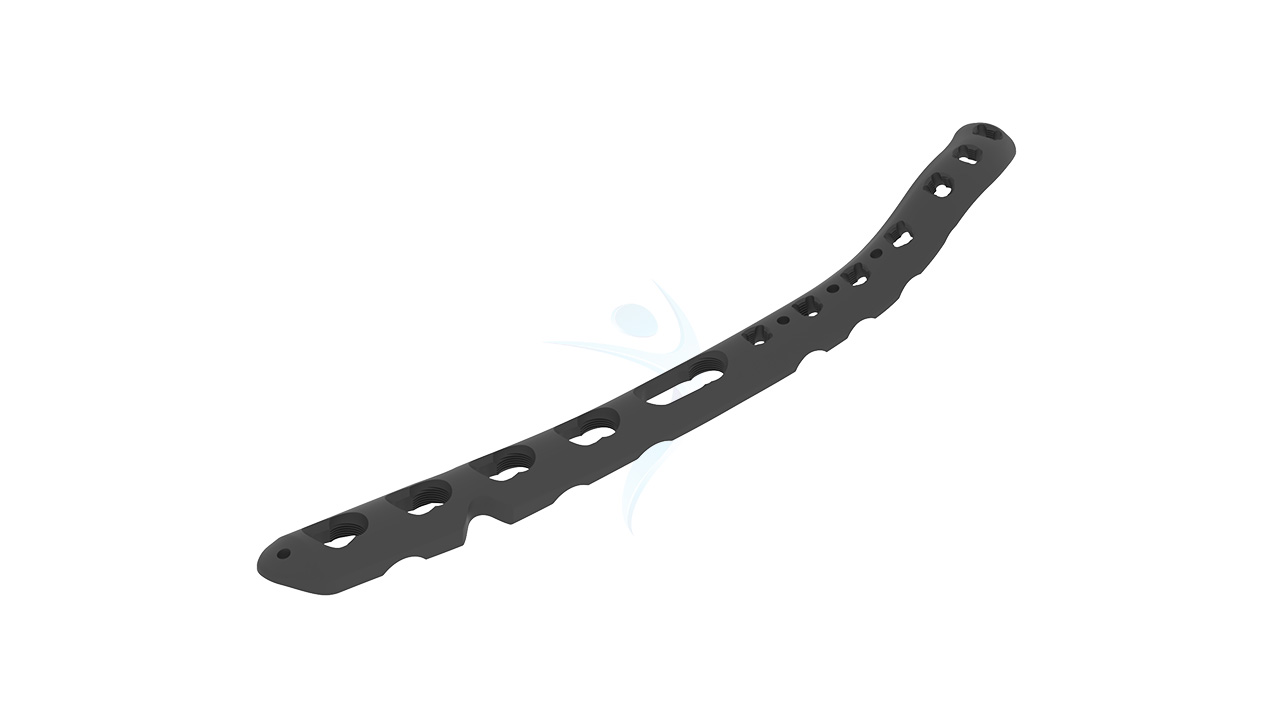
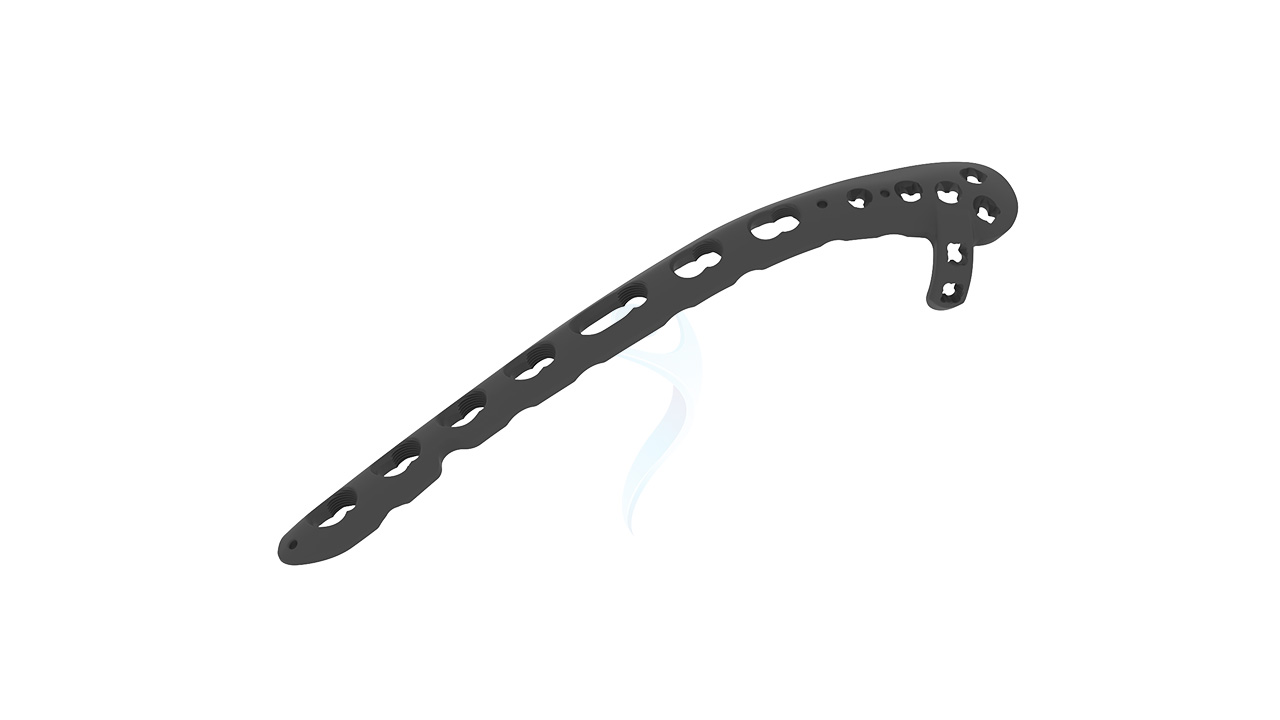
Distal Humerus Plate (VALP)- 2.7 / 3.5 Medial
Product Overview
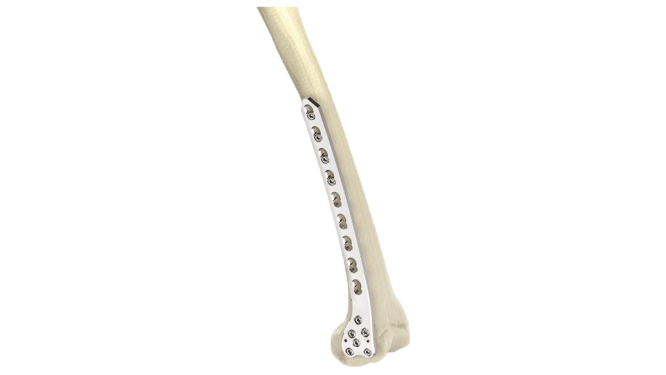
The 2.7 / 3.5 Distal Humerus Medial Plate (VALP) is a cutting-edge orthopedic implant designed for superior fixation of distal humerus fractures. Crafted with precision engineering and advanced materials, it offers optimal stability and support for efficient healing. Its anatomical design ensures proper alignment and distribution of forces, while its versatile screw options allow for tailored fixation. Trust in VALP for reliable performance and patient satisfaction in orthopedic care.







Product Uses
- Distal Humerus Fractures : Provides stable fixation for fractures at the distal end of the humerus, ensuring proper alignment and support for optimal healing.
- Osteotomies : Facilitates precise osteotomies of the distal humerus with reliable fixation, aiding in corrective surgeries.
- Non-union or Malunion Correction : Corrects non-union or malunion of distal humerus fractures by securely stabilizing the bone fragments.
- Revision Surgeries : Used in revision surgeries to address failed previous fixations or complications in distal humerus fractures.
- Trauma Cases : Suitable for traumatic injuries involving the distal humerus, offering dependable fixation to restore function and stability.
- Orthopedic Reconstruction : Integral in orthopedic reconstruction procedures aiming to restore the integrity and function of the elbow joint.
Product Specification
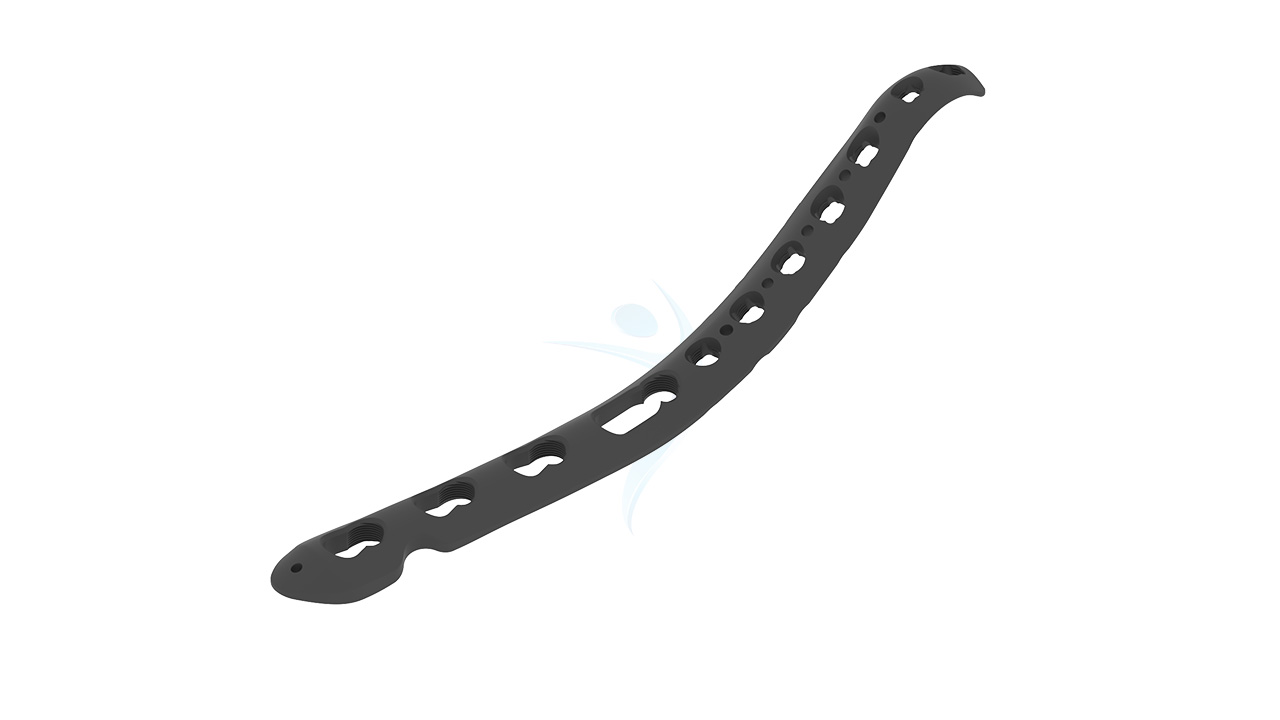
- Size Options : Available in 2.7 mm and 3.5 mm thickness options to accommodate different bone densities and fracture patterns.
- Material : Available in 2.7 mm and 3.5 mm thickness options to accommodate different bone densities and fracture patterns.
- Anatomical Design : Features an anatomically contoured shape to match the distal humerus anatomy, minimizing soft tissue irritation and optimizing bone contact for enhanced stability.
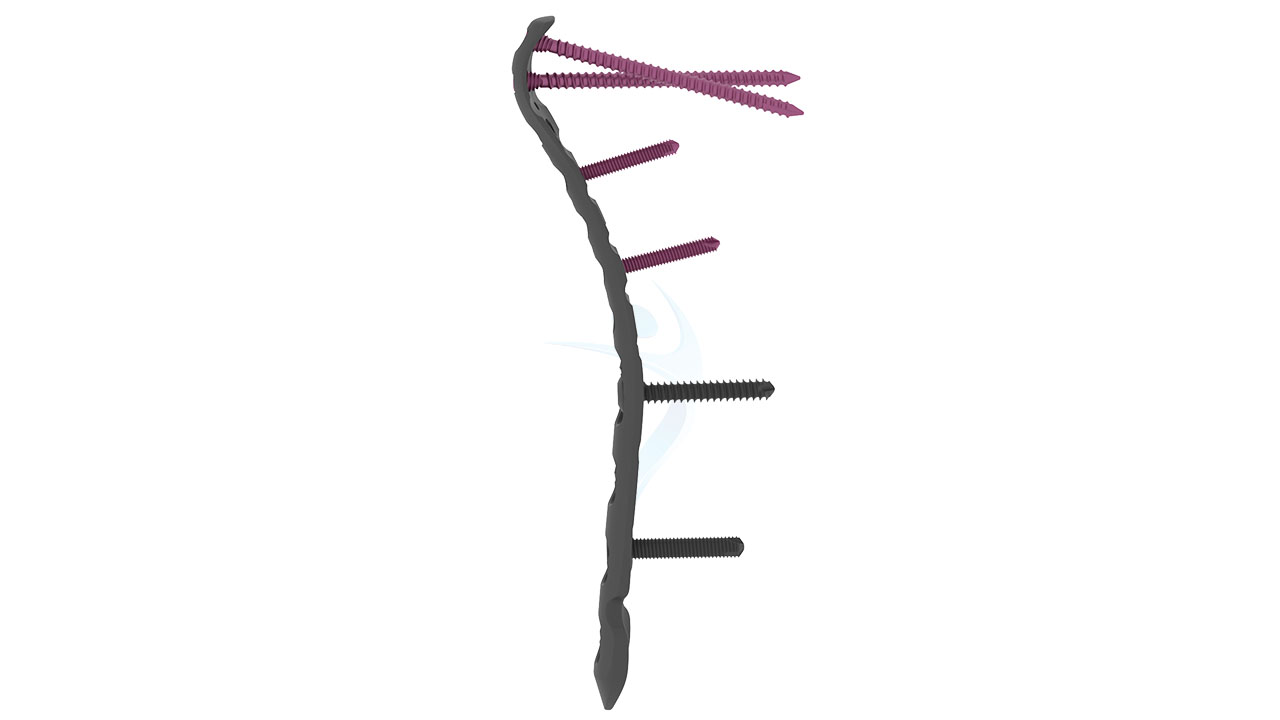
- Screw Holes : Multiple screw holes along the plate allow for versatile screw placement, enabling customized fixation based on fracture patterns and bone quality.
- Locking Mechanism : Incorporates locking screw technology for enhanced stability and angular stability, reducing the risk of screw loosening or backing out.
Distal Humerus Plate (VALP)- 2.7 / 3.5 Medial Sizes
Comprehensive Guide for Distal Humerus Plate (VALP)- 2.7 / 3.5 Medial
- Patient Evaluation : Review the patient's medical history, perform a physical examination, and assess imaging studies (X-rays, CT scans) to evaluate the distal humerus fracture.
- Surgical Planning : Analyze the fracture pattern and determine the appropriate size of the 2.7 / 3.5 Distal Humerus Medial Plate - VALP, as well as the number and placement of screws required for fixation.
- Informed Consent : Discuss the surgical procedure, potential risks, benefits, and alternatives with the patient, ensuring informed consent.
- Pre-operative Optimization : Optimize the patient's medical condition, including managing comorbidities, adjusting medications, and addressing any nutritional deficiencies.
- Antibiotic Prophylaxis : Administer prophylactic antibiotics according to institutional guidelines to reduce the risk of surgical site infection.
- Skin Preparation : Cleanse the surgical site with antiseptic solution to minimize the risk of contamination.
- Anesthesia : Collaborate with the anesthesia team to determine the appropriate anesthesia technique for the patient.
- Patient Positioning : Position the patient supine or in a lateral decubitus position, with the affected arm on a hand table or arm board.
- Incision : Make an appropriate incision over the distal humerus to expose the fracture site while preserving soft tissue integrity.
- Fracture Reduction : Carefully manipulate the fracture fragments into proper alignment using bone clamps, reduction forceps, or other reduction techniques.
- Plate Placement : Select the correct size and shape of the 2.7 / 3.5 Distal Humerus Medial Plate - VALP and position it on the medial aspect of the distal humerus.
- Screw Fixation : Secure the plate to the bone using locking or non-locking screws, ensuring adequate fixation and stability.
- Wound Closure : Close the incision in layers, ensuring hemostasis and meticulous closure of the subcutaneous and skin layers.
- Dressing Application : Apply a sterile dressing over the surgical site to protect the wound and minimize the risk of infection.
- Pain Management : Provide appropriate pain relief to ensure patient comfort.
- Early Mobilization : Encourage early mobilization and range of motion exercises under the guidance of a physiotherapist.
- Wound Care : Instruct the patient on proper wound care, including keeping the incision site clean and dry, and monitoring for signs of infection.
- Follow-up : Schedule follow-up appointments to monitor the patient's progress, assess healing, and remove sutures or staples as necessary.
- Rehabilitation : Implement a comprehensive rehabilitation program focused on restoring strength, mobility, and function of the elbow joint.
- Activity Restrictions : Advise the patient on activity restrictions to prevent implant failure or complications.








.png)