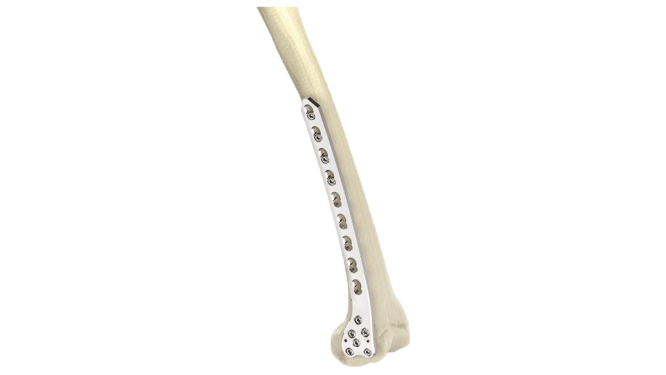
Proximal Femoral Nail Antirotation (PFNA) - Long & Short
Product Overview
The Proximal Femoral Nail Antirotation (PFNA) - Long & Short is an advanced orthopedic implant meticulously designed to offer unparalleled stability and support for treating proximal femoral fractures. Crafted from high-quality titanium, the PFN-A ensures superior biocompatibility and strength, facilitating optimal healing and enhanced patient comfort. Its versatile design and cutting-edge locking mechanisms provide precise fixation and rotational stability, resulting in accelerated recovery and improved treatment outcomes. Trust in the reliability and innovation of our PFN-A to meet your patients' orthopedic needs with utmost confidence.







Product Uses
- Intertrochanteric Fractures:The PFN-A is frequently used to treat intertrochanteric fractures, which are fractures that occur between the greater trochanter and the lesser trochanter of the femur.
- Subtrochanteric Fractures: It is also employed for subtrochanteric fractures, which are fractures that occur just below the lesser trochanter of the femur.
- Stable Fractures: The PFN-A is suitable for treating stable fractures, where the fractured bone ends are relatively well-aligned and stable.
- Unstable Fractures: In some cases of unstable fractures, the PFN-A can provide better stability and support, allowing for early mobilization and faster recovery.
- Comminuted Fractures:It is used for fractures with multiple bone fragments, providing stable fixation for proper healing.
- Revision Surgery: The PFN-A can be used in revision surgeries to treat complications from previous implant placements or fractures.
Product Specification
- Material:Made from high-quality medical-grade titanium alloy for strength and biocompatibility.
- Design:Intramedullary nail design specifically shaped to fit the proximal part of the femur, providing rotational stability and fixation.
- Nail Length: Different nail lengths available to accommodate various patient anatomies and fracture patterns.
- Diameter: Various nail diameters to match the medullary canal size of the femur.
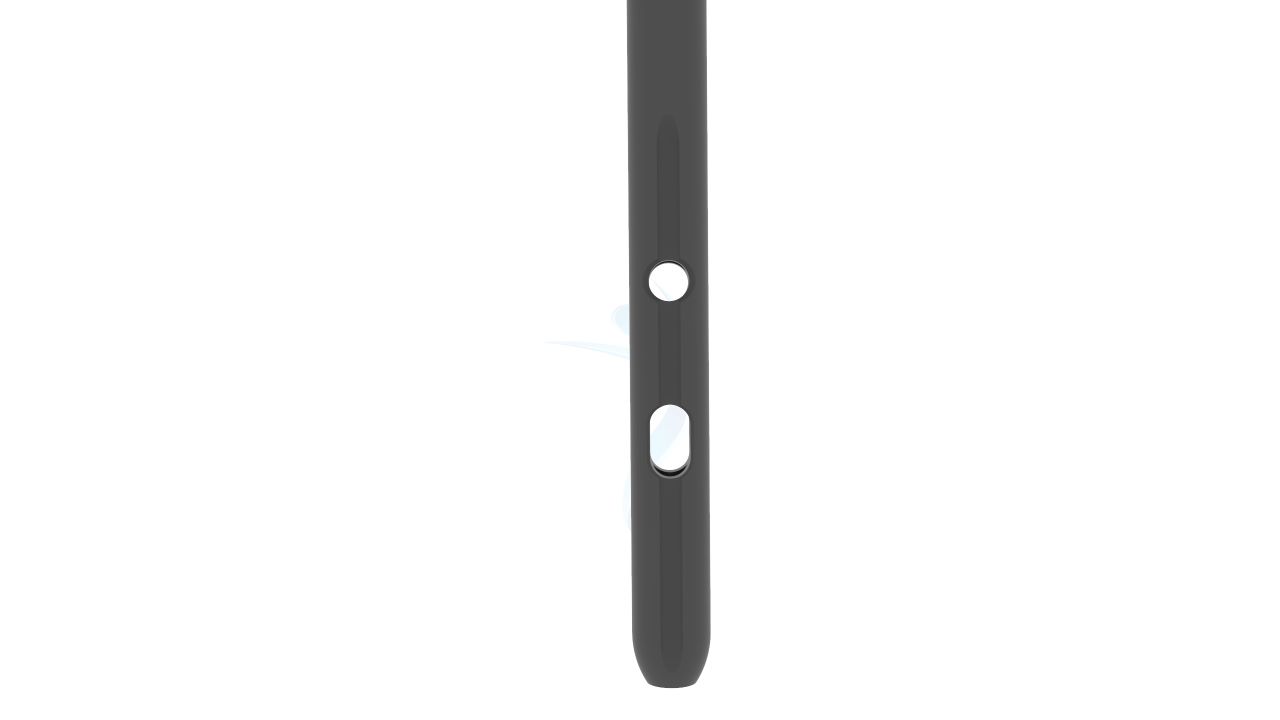
- Locking Mechanism: The nail may feature proximal locking options to prevent rotation and maintain stability.
- Distal Options: Some PFN-A models offer distal interlocking options for additional stability in certain fracture patterns.
Proximal Femoral Nail Antirotation (PFNA) - Long & Short Sizes
Comprehensive Guide for Proximal Femoral Nail Antirotation (PFNA) - Long & Short
- Medical evaluation:The patient's medical history, including any previous surgeries, allergies, and chronic medical conditions, is reviewed. Preoperative tests, such as blood tests, X-rays, and possibly a CT scan or MRI, may be conducted to assess the extent and characteristics of the fracture.
- Preoperative counseling : The patient is informed about the surgical procedure, its risks, benefits, and expected outcomes. The surgeon will discuss the specific details of the surgery, including the type of implant (Proximal Femur Nail Antirotation) and potential complications.
- Medications and allergies : The patient should inform the surgical team about any medications they are taking, including prescription drugs, over-the-counter medications, and supplements.
- Fasting instructions : The patient will receive specific instructions regarding fasting before the surgery, typically requiring abstaining from food and drink (including water) for a specified period before the procedure.
- Anesthesia consultation : If general anesthesia is planned, the patient may undergo a preoperative anesthesia consultation to evaluate their fitness for anesthesia and to discuss anesthesia options and potential risks.
- Anesthesia : The patient is typically placed under general anesthesia, although regional anesthesia (e.g., spinal or epidural) may also be used depending on the patient's condition and the surgeon's preference. The chosen anesthesia method will ensure that the patient remains comfortable and pain-free throughout the procedure.
- Patient positioning : The patient is positioned on the operating table, usually lying on their back. The affected leg is appropriately positioned and prepped to provide optimal access to the proximal femur.
- Incision : The surgeon makes an incision over the proximal femur region. The location and length of the incision may vary depending on the specific fracture pattern and the implant design.
- Soft tissue management : The surrounding soft tissues, such as muscles and tendons, are carefully dissected and retracted to expose the fractured area and the femur's medullary canal.
- Fracture reduction : The fractured fragments are then realigned (reduced) into their proper anatomical position. This may involve gentle manipulation, traction, or the use of specialized reduction instruments.
- Recovery and monitoring : The patient is taken to a recovery area where vital signs, pain levels, and any immediate postoperative complications are monitored.
- Pain management : Adequate pain control is essential for patient comfort and early mobilization. Pain medication may be administered through intravenous (IV) or oral routes as prescribed by the surgeon.
- Wound care : The surgical incision site should be kept clean and monitored for signs of infection. Dressings may be changed regularly, following the surgeon's instructions.
- Early mobilization and weight-bearing : Depending on the specific fracture and the surgeon's instructions, early mobilization and partial weight-bearing may be initiated.
- Physical therapy and rehabilitation : A structured physical therapy program is crucial for the patient's long-term recovery. Physical therapists will provide exercises and rehabilitation techniques to restore strength, range of motion, and functional mobility.





.png)