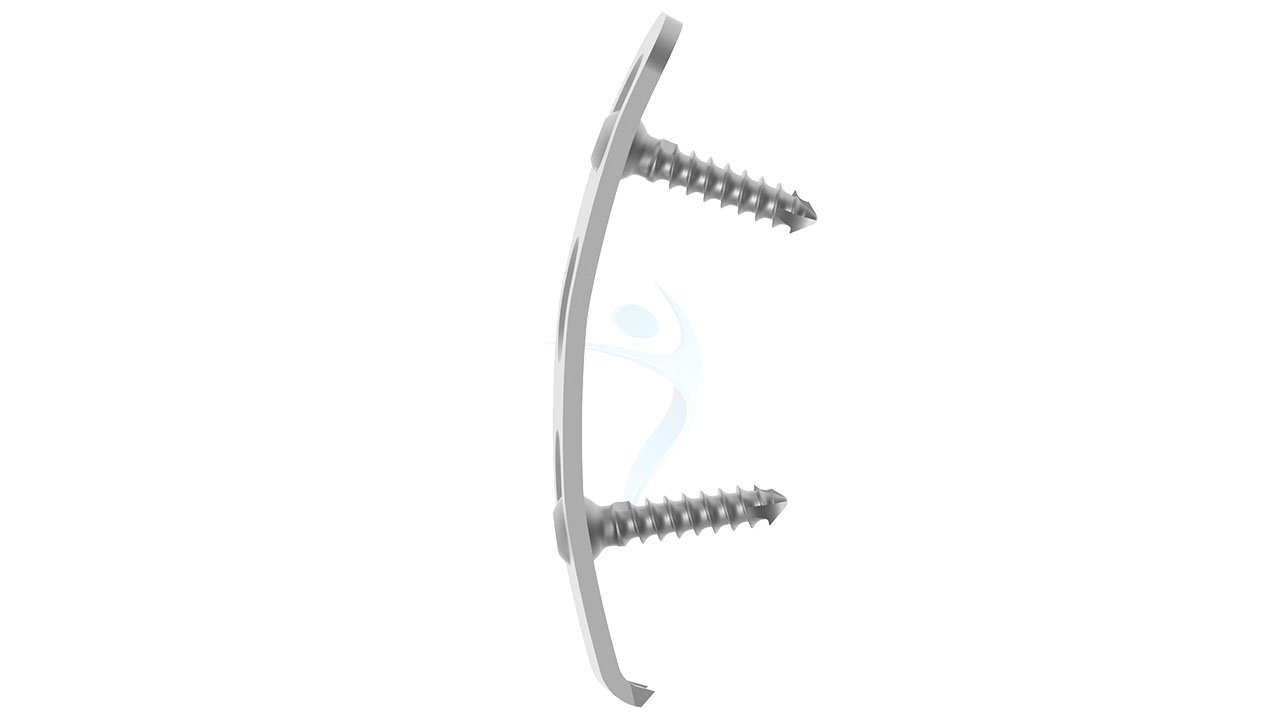
Pelvic Plate - 3.5 mm Spring (Reconstrcution)
Product Overview
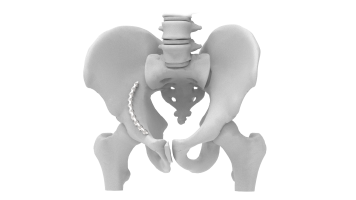
The 3.5 mm Spring Pelvic Plate is a high-quality orthopedic implant designed to provide stability and support for pelvic fractures. Made from biocompatible materials, this plate ensures optimal bone healing and reconstruction. Its 3.5 mm thickness offers a robust yet low-profile solution for various fracture types, making it ideal for complex pelvic surgeries. The spring design allows for flexibility and precise anatomical alignment, enhancing patient recovery and mobility. Suitable for use in orthopedic trauma procedures, this implant aids in restoring pelvic integrity and function effectively.





Product Uses
- Pelvic Fracture Stabilization : Provides robust stabilization for fractured pelvic bones, ensuring proper alignment and promoting efficient healing.
- Pelvic Reconstruction : Aids in reconstructing the pelvic anatomy following traumatic injuries, ensuring structural integrity and functional recovery.
- Treatment of Acetabular Fractures : Suitable for fixing fractures in the acetabulum, helping to restore hip joint stability.
- Complex Pelvic Surgery : Utilized in complex pelvic surgeries where precise anatomical alignment and flexibility are crucial.
- Post-Trauma Support : Offers long-term support to the pelvic region after severe trauma, preventing complications and promoting rehabilitation.
- Orthopedic Trauma Procedures : Used in various orthopedic trauma procedures involving the pelvis, providing reliable fixation and support.
Product Specification
- Material : High-grade stainless steel or titanium for biocompatibility and durability.
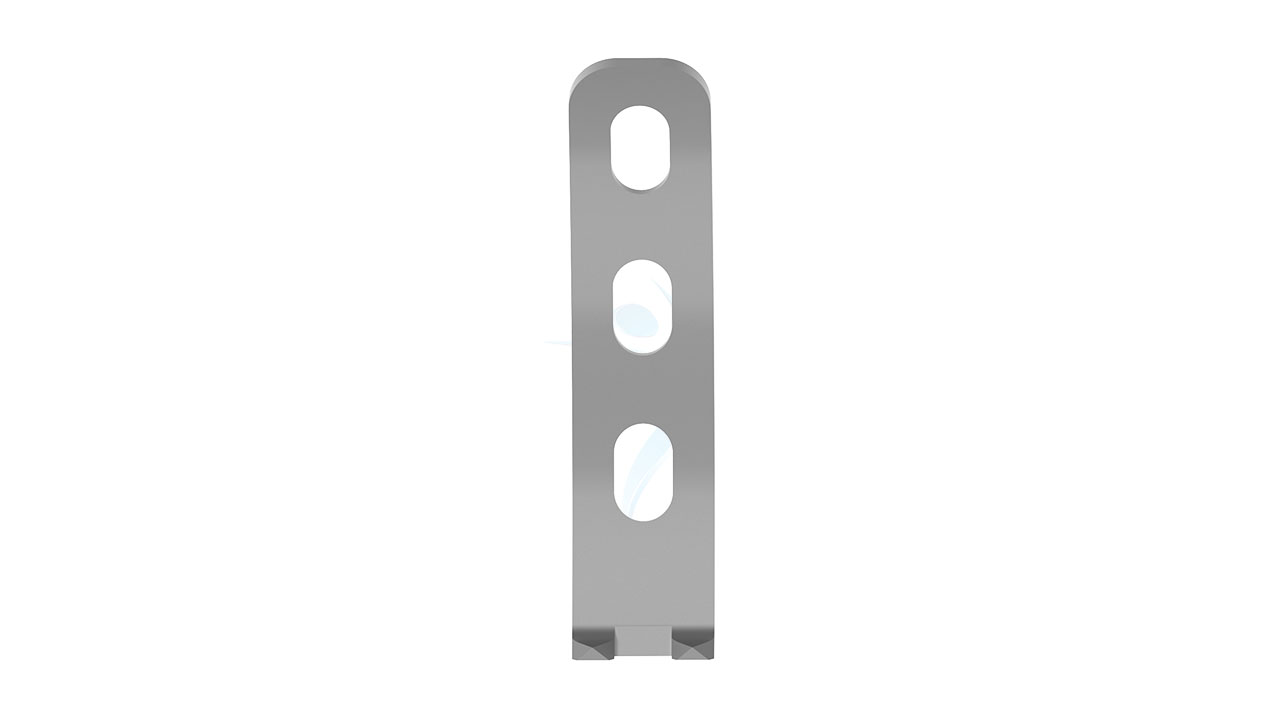
- Thickness : 3.5 mm, providing a balance between strength and a low profile.
- Length : Available in various lengths to accommodate different fracture patterns and patient anatomies.
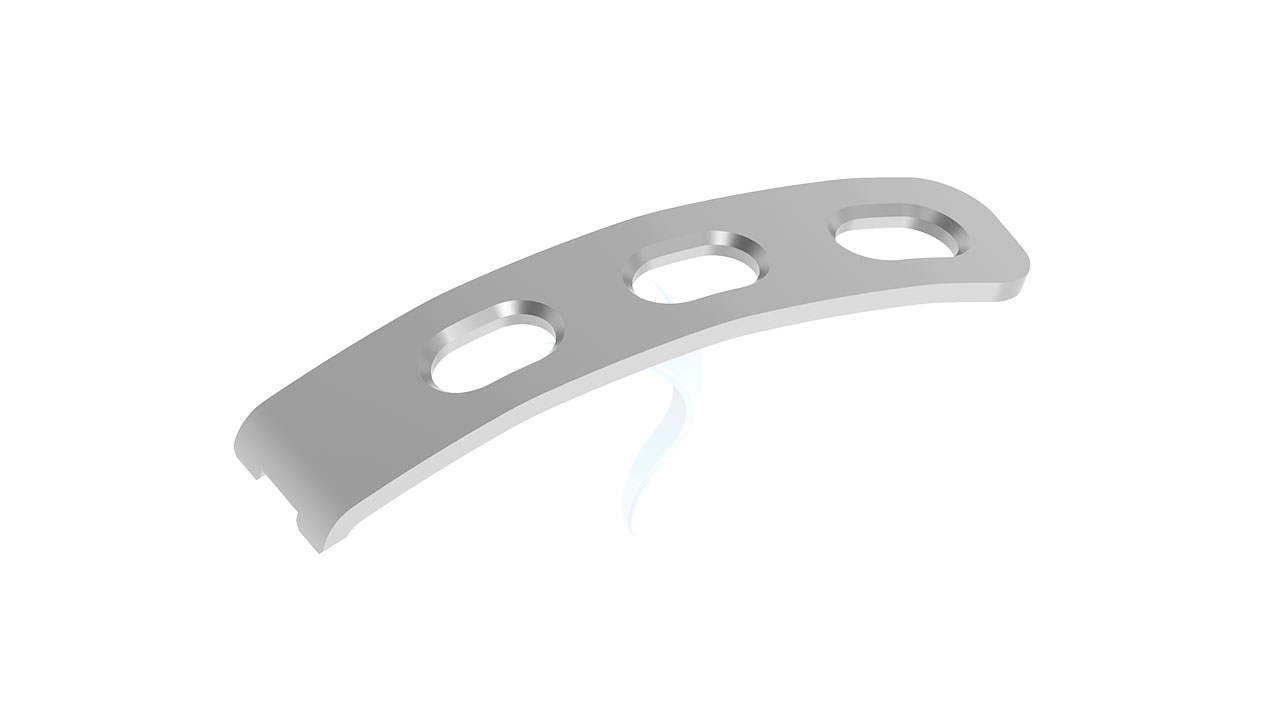
- Design : Spring design for flexibility and precise anatomical alignment, allowing for better conformance to the pelvic curvature.
- Width : Standard width suitable for pelvic fixation.
- Screw Holes : Multiple screw holes along the plate for secure fixation; compatible with 3.5 mm cortical screws.
- Surface Finish : Smooth, polished surface to minimize tissue irritation and promote bone healing.
Pelvic Plate - 3.5 mm Spring Sizes
Comprehensive Guide for Pelvic Plate - 3.5 mm Straight
- Patient Assessment : Thoroughly evaluate the patient's medical history, including any prior surgeries, allergies, medications, and comorbidities. Conduct a physical examination to assess the overall health and specific condition of the pelvic fracture.
- Imaging Studies : Obtain detailed imaging studies such as X-rays, CT scans, or MRI to evaluate the extent and specifics of the pelvic fracture. Use these images to plan the surgical approach and determine the exact size and positioning of the implant.
- Surgical Planning : Develop a detailed surgical plan, including the selection of the appropriate length of the 3.5 mm Spring Pelvic Plate and the fixation points.
- Patient Preparation : Administer prophylactic antibiotics and other pre-operative medications as required. Mark the surgical site and anatomical landmarks to guide the incision and implant placement.
- Instrument Preparation : Ensure all necessary surgical instruments, implants, and equipment are sterilized and ready for use.
- Anesthesia : Administer appropriate anesthesia (general or regional) based on patient needs and surgical requirements.
- Incision : Make a precise surgical incision to access the pelvic fracture site. The incision should provide adequate exposure while minimizing tissue damage.
- Fracture Reduction : Carefully manipulate the bone fragments to achieve proper alignment and anatomical restoration of the pelvis.
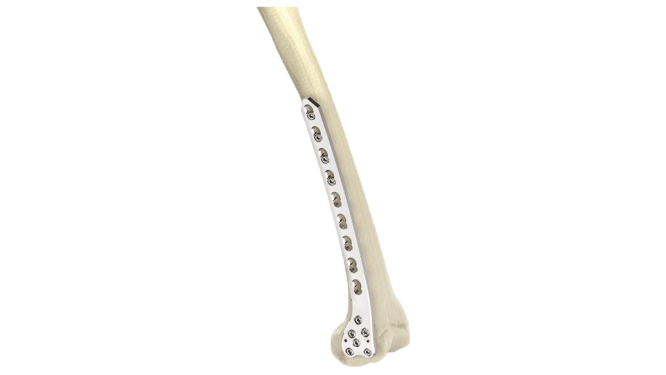
- Plate Placement :Position the 3.5 mm Spring Pelvic Plate over the fracture site, ensuring it conforms to the pelvic anatomy. Ensure the spring design allows for flexibility and proper alignment with the bone structure.
- Screw Fixation : Secure the plate to the bone using appropriate screws through the pre-drilled holes in the plate. Verify that the screws are placed correctly and the plate is firmly anchored.
- Monitoring : Closely monitor the patient in the recovery room for any immediate postoperative complications such as bleeding, infection, or nerve injury.
- Pain Management : Provide adequate pain relief through medications and other pain management techniques to ensure patient comfort.
- Physical Therapy : Initiate early mobilization and physical therapy as tolerated to prevent stiffness, promote healing, and regain strength and function.
- Follow-up : Schedule regular follow-up visits to monitor the patient's progress, assess the healing of the fracture, and check the integrity of the implant.
- Activity Restrictions : Advise the patient on activity modifications and restrictions to avoid putting excessive stress on the pelvic region during the healing process.







.png)