Pelvic Plate - 3.5 mm Straight (Reconstrcution)
Product Overview
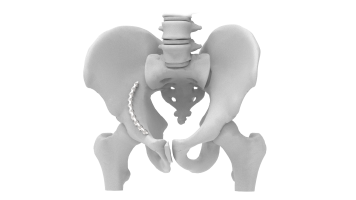
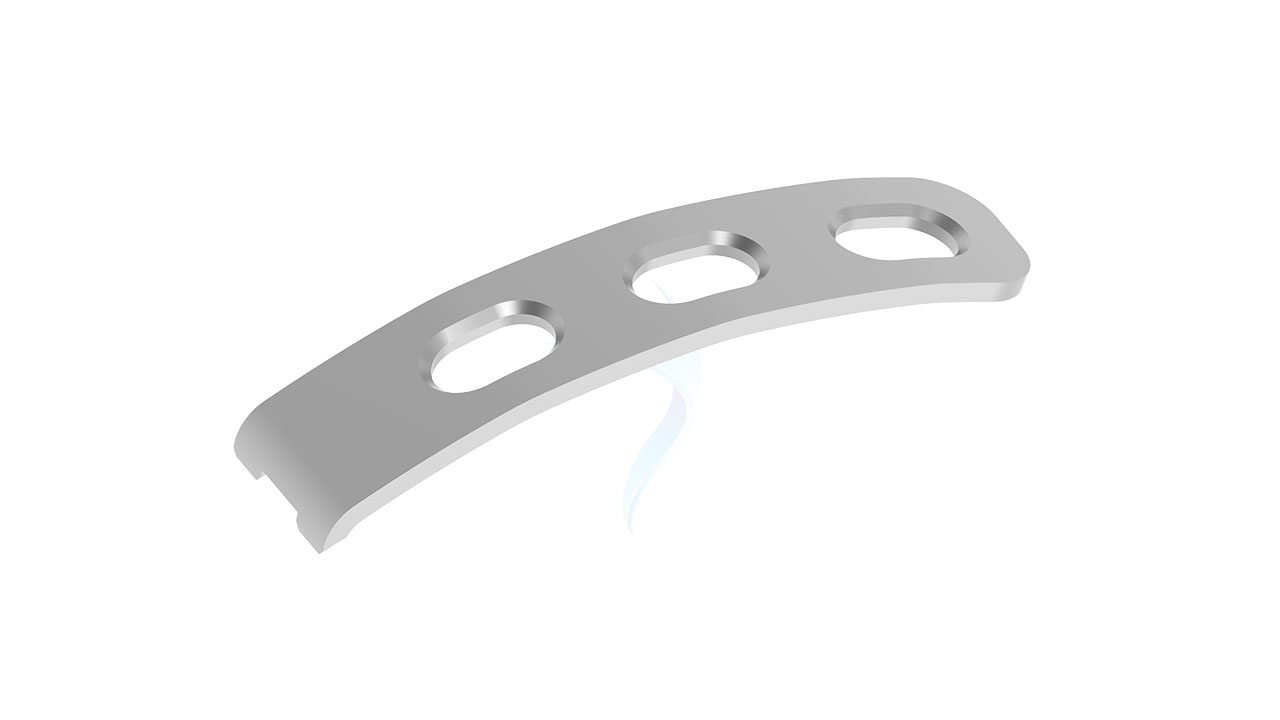
The 3.5 mm Straight Pelvic Plate is a high-quality orthopedic implant designed for the surgical fixation and stabilization of pelvic fractures. Crafted from durable, biocompatible materials, this plate provides optimal support for bone healing and alignment. Its straight design allows for precise reconstruction of complex pelvic anatomy, ensuring stability and reducing recovery time. The 3.5 mm thickness offers a balance of strength and minimal profile, making it suitable for various fracture types. Ideal for orthopedic surgeons, this implant enhances patient outcomes and facilitates quicker return to mobility.






Product Uses
- Pelvic Fracture Fixation : It is primarily used to stabilize and support fractured pelvic bones, providing structural integrity to the pelvic region.
- Pelvic Reconstruction : The plate aids in reconstructing and restoring the normal anatomy of the pelvis following traumatic injuries or deformities.
- Fracture Reduction : By securely fixing the fractured bones in proper alignment, it facilitates the reduction of pelvic fractures, promoting optimal healing.
- Orthopedic Surgery :Utilized in complex orthopedic surgeries where precise fixation and durability are required.
- Post-Trauma Support : Offers support and reinforcement to the pelvic region after traumatic injuries.
- Treatment of Complex Pelvic Injuries : It is employed in the management of complex pelvic fractures, including those involving the acetabulum and sacrum.
Product Specification
- Material : Manufactured from medical-grade stainless steel or titanium alloy for biocompatibility and durability.
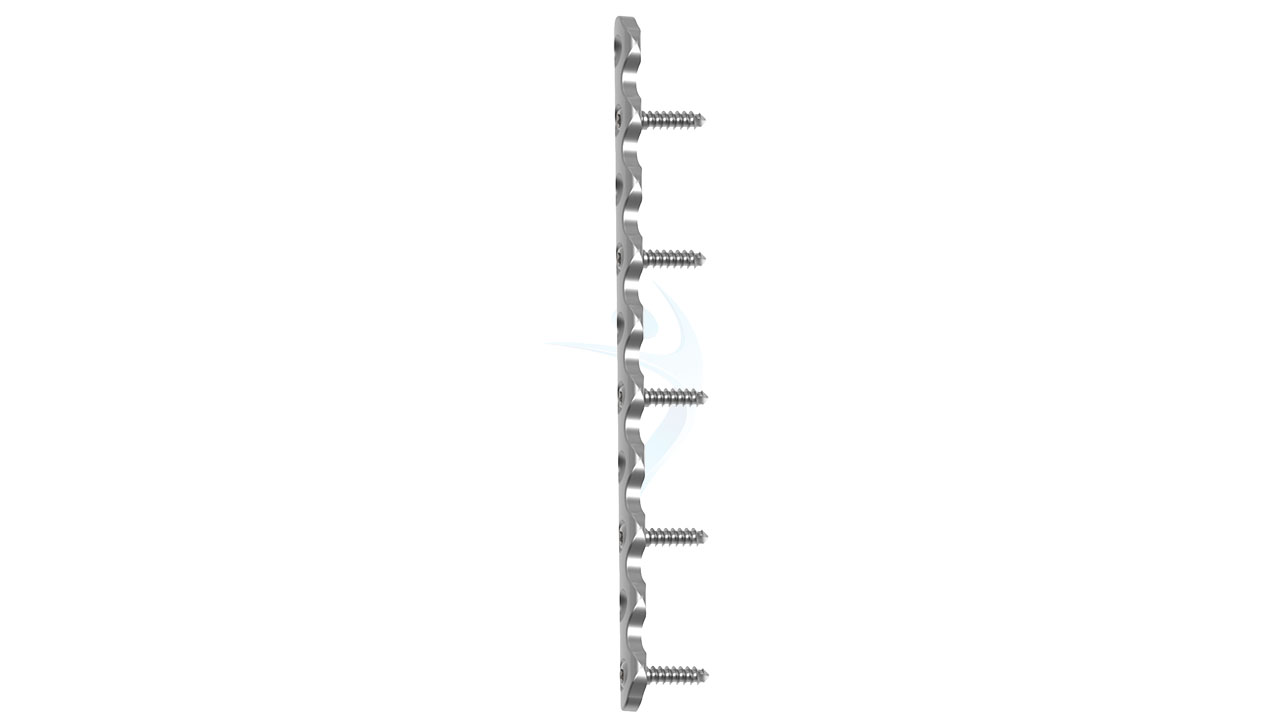
- Thickness : 3.5 mm, providing a balance between strength and low profile.
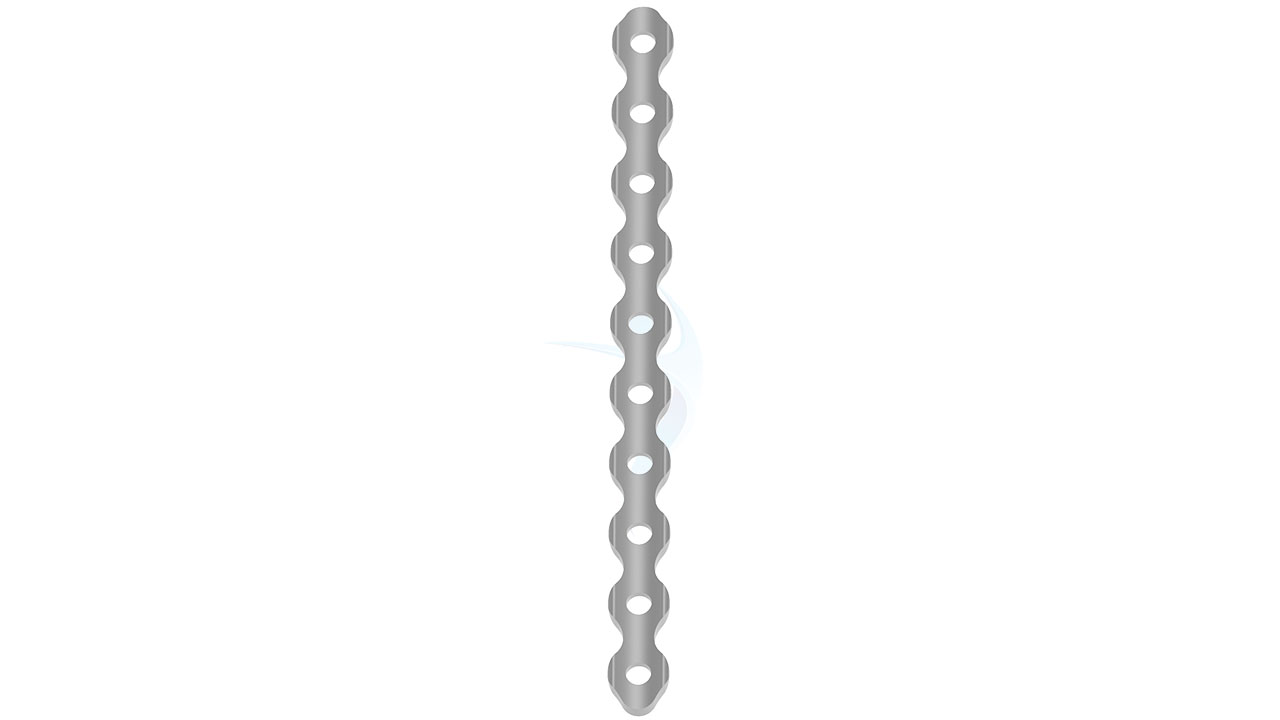
- Design : Straight plate design for versatile application and precise reconstruction of pelvic anatomy.
- Width : Standard width suitable for pelvic fixation and stabilization.
- Length : Available in various lengths to accommodate different patient anatomies and fracture patterns.
- Holes : Multiple screw holes along the plate for secure fixation to the bone.
- Surface : Smooth surface finish to minimize tissue irritation and promote bone healing.
Pelvic Plate - 3.5 mm Straight Sizes
Comprehensive Guide for Pelvic Plate - 3.5 mm Straight
- Patient Evaluation : Assess the patient's medical history, current condition, and any associated injuries or comorbidities.
- Imaging Studies : Conduct imaging studies such as X-rays, CT scans, or MRI to assess the extent and nature of the pelvic fracture.
- Surgical Planning : Plan the surgical approach, including the selection of appropriate plate size and fixation points based on the fracture pattern and patient anatomy.
- Informed Consent : Obtain informed consent from the patient after discussing the surgical procedure, risks, benefits, and potential complications.
- Patient Positioning : Position the patient appropriately on the operating table, ensuring access to the surgical site and optimal visualization for the surgical team.
- Anesthesia : Administer appropriate anesthesia, either general or regional, based on the patient's condition and surgeon preference.
- Incision : Make an appropriate surgical incision, typically in the pelvic region, to access the fractured bones.
- Fracture Reduction : Reduce the fracture by manipulating the bone fragments into proper alignment, ensuring anatomical restoration.
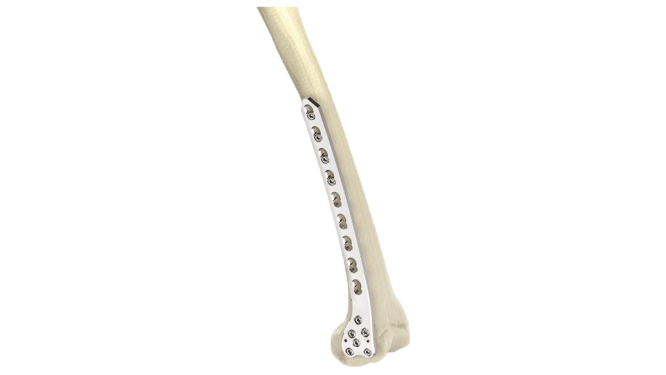
- Plate Placement : Position the 3.5 mm Straight Pelvic Plate over the fracture site, aligning it properly with the bone surface.
- Screw Fixation : Secure the plate to the bone using screws inserted through the plate's screw holes, ensuring stable fixation.
- Monitoring : Monitor the patient closely in the recovery room for any signs of complications such as bleeding, infection, or nerve injury.
- Pain Management : Provide adequate pain management to ensure patient comfort and facilitate early mobilization.
- Physical Therapy : Initiate early mobilization and physical therapy as tolerated to prevent stiffness, promote healing, and regain strength.
- Follow-up : Schedule regular follow-up appointments to assess the progress of healing, monitor implant integrity, and address any concerns.
- Activity Modification : Instruct the patient on activity modification and restrictions to avoid excessive stress on the pelvic region during the healing process.






.png)