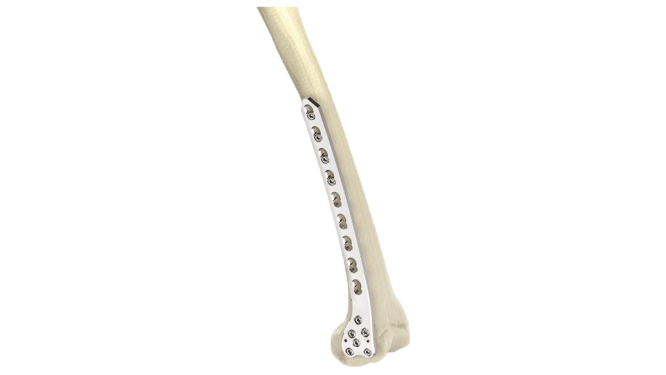
Distal Humerus Plate (ASLP)- 3.5 mm Metaphyseal
Product Overview
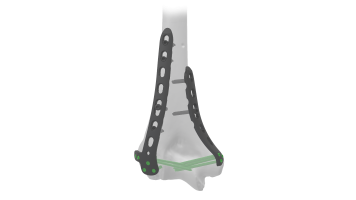
Introducing the ASLP - 3.5 Metaphyseal Plate for Distal, Medial Humerus, a cutting-edge orthopedic implant designed to revolutionize the treatment of fractures and deformities in the humerus bone. Crafted with precision and innovation, this plate offers unparalleled support and stability, ensuring optimal healing and restoration of function for patients.The ASLP - 3.5 Metaphyseal Plate boasts a meticulously engineered design, specifically tailored to address the unique anatomical challenges of the distal, medial humerus.




Product Uses
- Fracture Fixation : The plate is used to stabilize and align fractures of the distal or medial humerus, providing immediate support to the bone fragments and promoting proper healing.
- Osteotomies : Surgeons utilize the ASLP - 3.5 Plate to perform corrective osteotomies, restoring proper alignment and function to the humerus in cases of malunion, nonunion, or deformities such as cubitus varus or valgus.
- Joint Reconstruction : In cases of severe joint damage or instability, the plate can be employed as part of a joint reconstruction procedure, providing structural support to the humeral head and facilitating joint stability and mobility.
- Nonunion Repair : The ASLP - 3.5 Plate aids in the repair of nonunions, where a fracture fails to heal properly, by providing rigid fixation and promoting bone union through the application of compression and stability.
- Tumor Resection : In cases of bone tumors or metastatic lesions affecting the distal or medial humerus, the ASLP - 3.5 Plate may be utilized to stabilize the bone following tumor resection, providing structural support and reducing the risk of pathological fractures.
- Revision Surgery : The plate can also be employed in revision surgeries to address complications or failures of previous hardware fixation, offering a reliable and adaptable solution for restoring stability and function to the humerus.
Product Specification
- Material : Manufactured from high-quality, medical-grade stainless steel or titanium alloy, ensuring excellent biocompatibility, corrosion resistance, and mechanical strength.
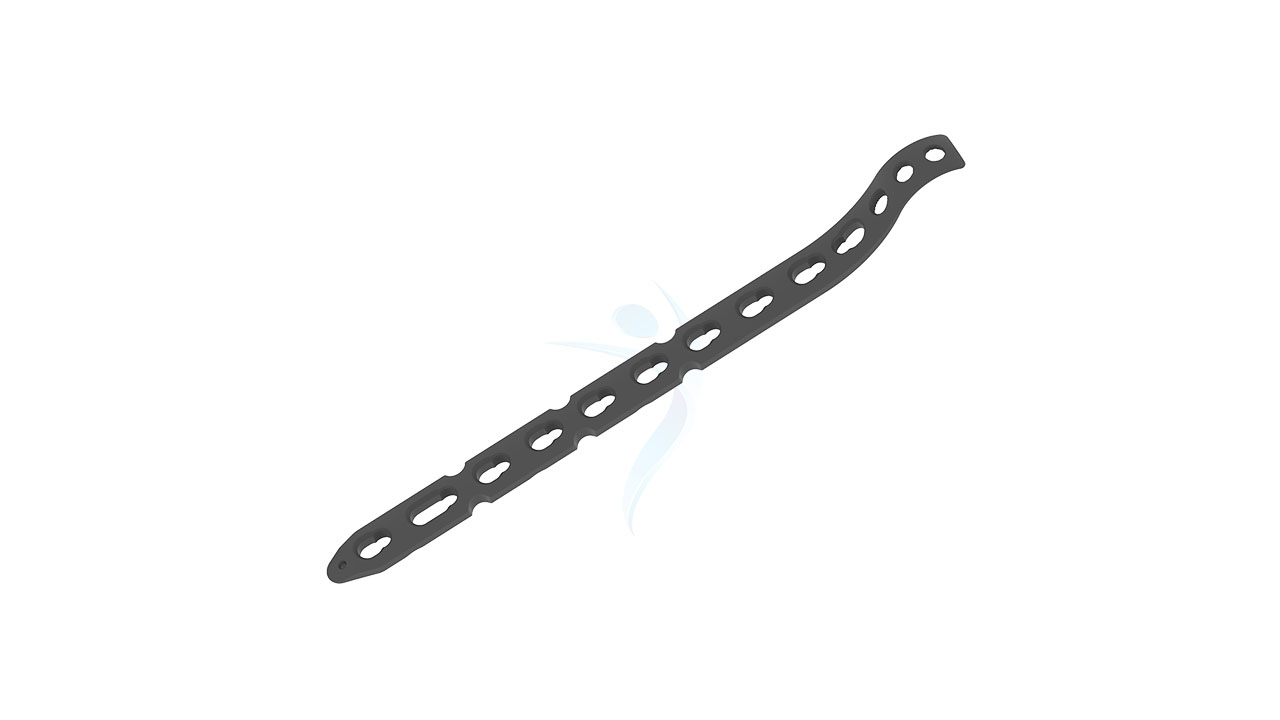
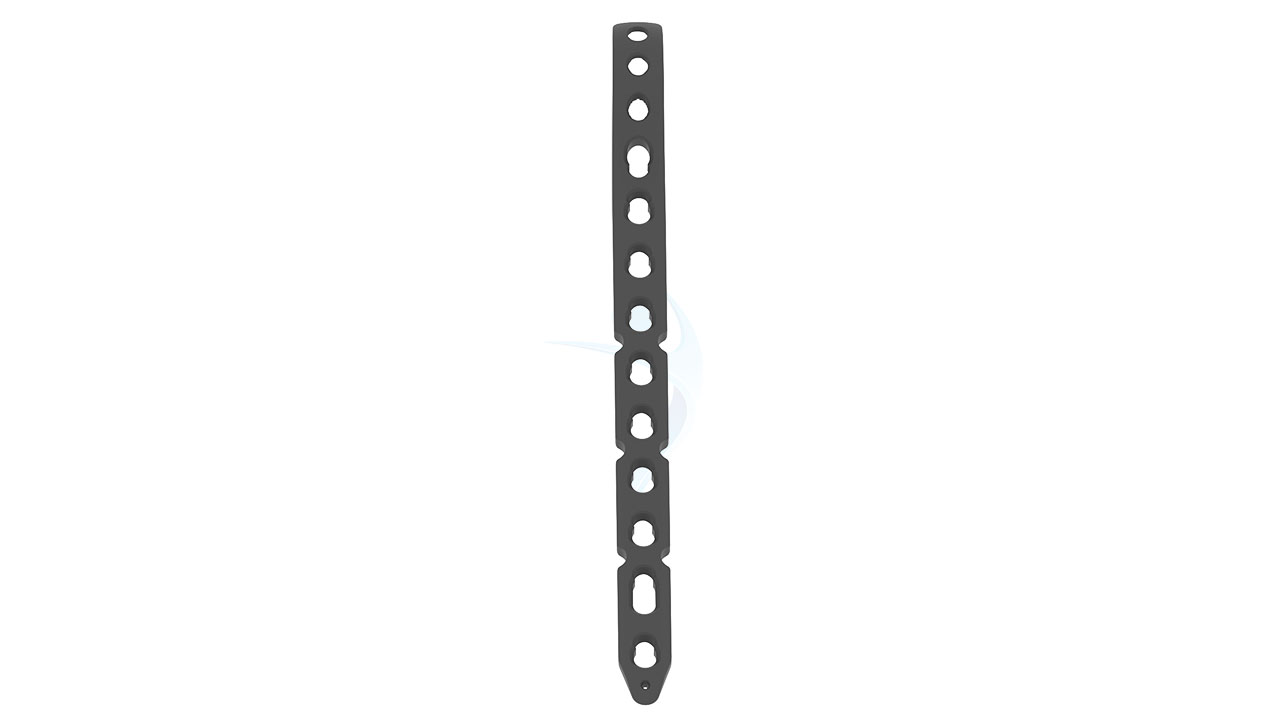
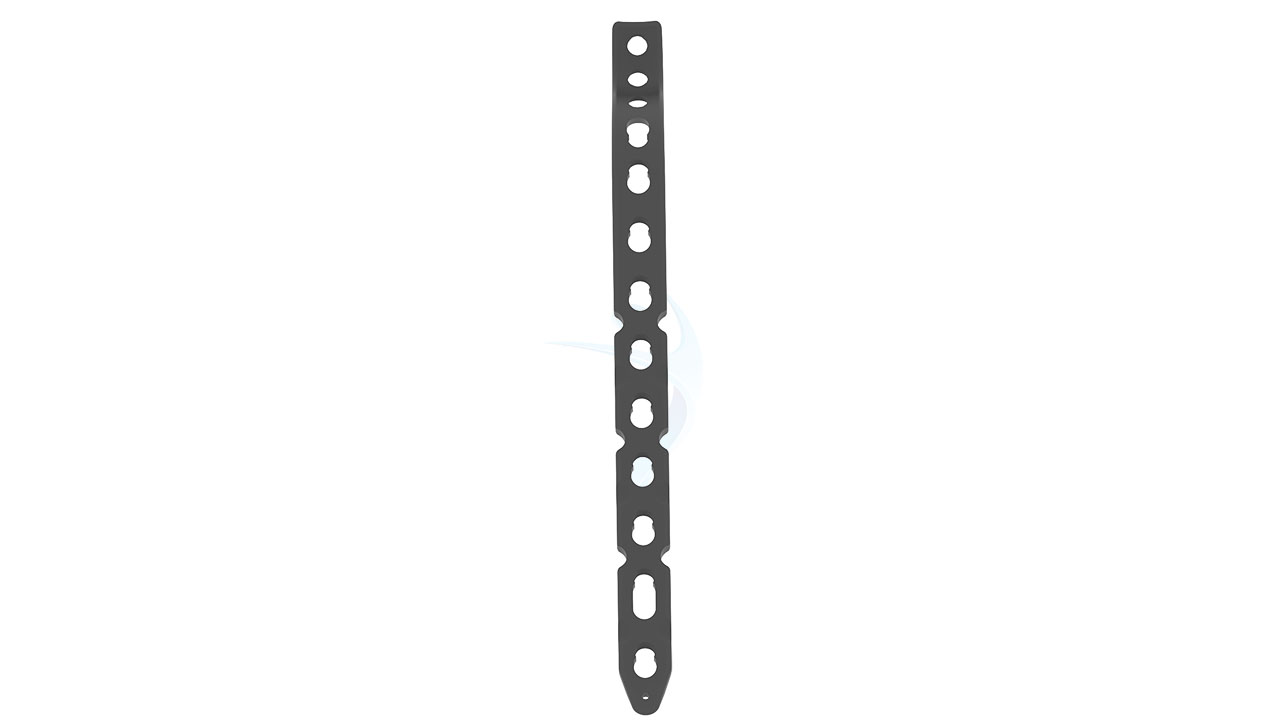
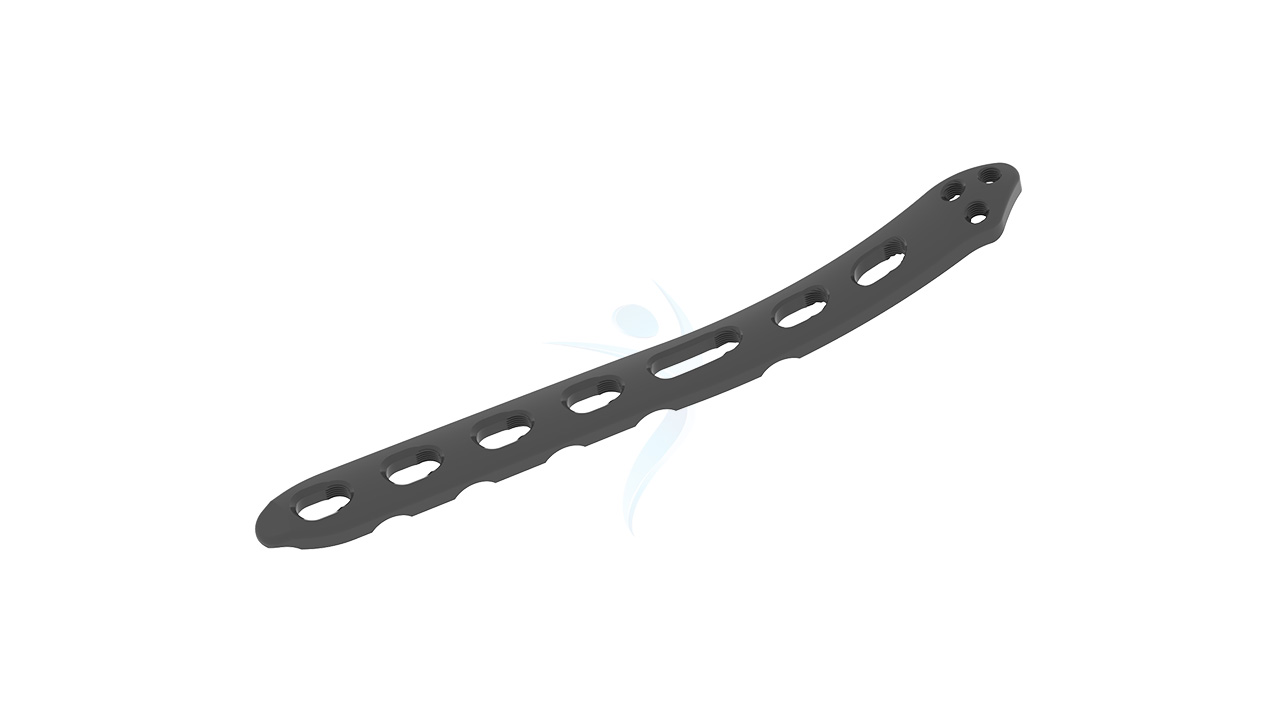
- Plate Type : Anatomically contoured plate designed specifically for the distal and medial regions of the humerus, featuring a low-profile design to minimize soft tissue irritation and optimize patient comfort.
- Plate Thickness : Approximately 3.5 mm, providing a balance between strength and flexibility to accommodate the biomechanical demands of the humeral bone while minimizing implant prominence.
- Plate Length : Available in various lengths to accommodate different patient anatomies and fracture patterns, typically ranging from approximately 80 mm to 180 mm.
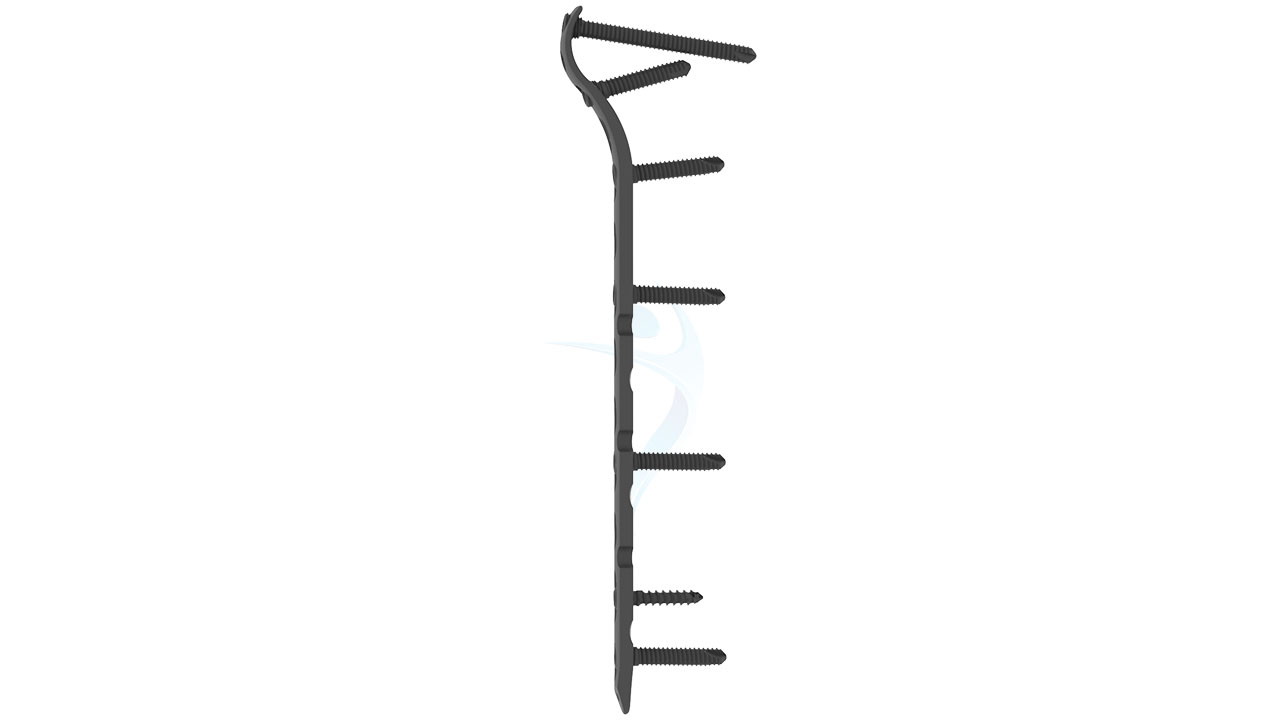
- Screw Holes : Multiple screw holes along the plate length, strategically positioned to allow for optimal fixation of bone fragments and promote stability during fracture reduction and fusion procedures.
- Locking Mechanism : Incorporates locking screw technology, enabling secure fixation and angular stability, particularly useful in osteoporotic bone or cases requiring enhanced biomechanical support.
Distal Humerus Plate (ASLP)- 3.5 mm Metaphyseal Sizes
Comprehensive Guide for Distal Humerus Plate (ASLP)- 3.5 mm Metaphyseal
- Patient Evaluation : Assess the patient's medical history, including any previous surgeries, allergies, medications, and underlying medical conditions. Conduct a physical examination and review imaging studies (X-rays, CT scans, MRI) to evaluate the extent of the fracture or condition affecting the distal or medial humerus.
- Surgical Planning : Collaborate with the surgical team to develop a comprehensive surgical plan tailored to the patient's specific needs and the nature of the injury or condition.
- Informed Consent : Obtain informed consent from the patient, discussing the risks, benefits, and alternatives of the procedure, including potential complications associated with the use of orthopedic implants such as the ASLP - 3.5 Plate.
- Preoperative Preparation :Instruct the patient on preoperative instructions, including fasting requirements, medication management, and personal hygiene. Ensure all necessary surgical instruments, implants, and equipment, including the ASLP - 3.5 Plate and associated screws, are prepared and sterilized according to established protocols.
- Anesthesia : Administer anesthesia according to the anesthesiologist's or surgeon's preference, typically general anesthesia or regional anesthesia with sedation, based on the patient's medical status and surgical requirements.
- Surgical Approach : Position the patient appropriately on the operating table and prepare the surgical site using aseptic techniques. Access the distal or medial humerus through the selected surgical approach, such as a deltopectoral or posterior approach, exposing the fracture or affected area while minimizing soft tissue trauma.
- Fracture Reduction : Carefully reduce the fracture fragments under direct visualization, using manual manipulation or specialized instruments as needed to restore proper alignment and anatomical congruence.
- Plate Placement : Select the appropriate size and contour of the ASLP - 3.5 Plate based on preoperative measurements and intraoperative assessment.
- Closure : Close the surgical incision in layers, meticulously approximating the soft tissues to minimize dead space and promote wound healing. Apply sterile dressings and immobilization devices, such as a sling or brace, as indicated based on the surgical technique and patient factors.
- Recovery and Monitoring : Transfer the patient to the recovery area for close monitoring of vital signs, pain management, and neurological status. Monitor for signs of complications, such as excessive bleeding, wound infection, or neurovascular compromise, and intervene promptly as needed.
- Physical Therapy : Initiate early mobilization and physical therapy under the guidance of a qualified therapist to promote joint mobility, muscle strength, and functional recovery. Provide instructions on home exercises and activity modifications to facilitate rehabilitation and prevent complications.
- Follow-Up Care : Schedule regular follow-up appointments with the surgeon to monitor the patient's progress, evaluate radiographic evidence of fracture healing, and adjust the treatment plan as necessary.
- Implant Removal : Depending on the patient's clinical course and preferences, consider the option of implant removal once the fracture has healed sufficiently and the bone has regained adequate strength. Discuss the risks and benefits of implant removal with the patient and make an informed decision based on individual circumstances.







.png)